MOST PRACTITIONERS today are becoming increasingly familiar with the concept of higher-order aberrations (HOAs). From reading about HOAs in the literature to testing out the newest aberrometer at a conference, there are ample opportunities to learn more about this hot topic in eyecare technology. However, when certain subjects start garnering more attention and popularity, it does beg the question, is this all it is cracked up to be?
Aberrations may be of a lower or higher order. Lower-order aberrations (LOAs) are what we consider as typical refractive error: myopia, hyperopia, and astigmatism. HOAs are any other components of the visual system that disrupt the path of light as it travels through the eye. HOAs cannot be corrected with standard glasses or contact lenses. They have been discussed for many years, and the concept has gained traction with the utilization of Zernike polynomials and really taken off due to the development of the Shack-Hartmann wavefront sensor (Howland and Howland, 1976; Liang et al, 1994).
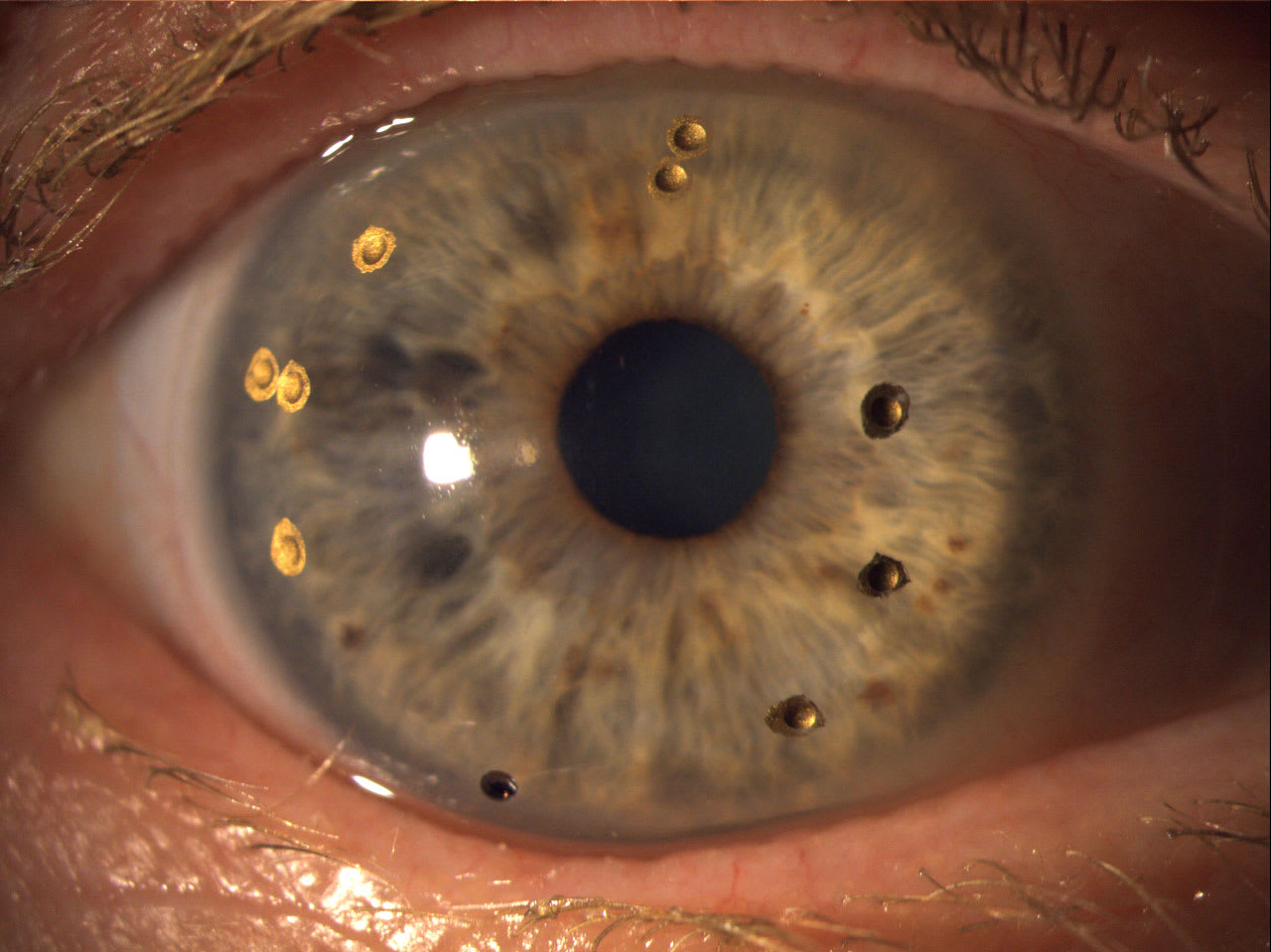
The vast majority of human eyes, including those of emmetropes, have HOAs to some degree. This does not mean that most patients need HOA-correcting contact lenses. Typically, patients who have corneal irregularities, ectasia, surgical history, trauma, or high ametropia do have bothersome HOAs (McCormick et al, 2005; Martínez-Pérez et al, 2024). Identifying patients who have significant HOAs can begin with a simple conversation; these patients may be 20/20, but not 20/happy.
Patients may be chasing perfection to enhance their sports game, attempting to max out their usable vision for work obligations, or simply looking for a way to improve their vision perception when things feel “off.” Regardless of the motivation, these patients often have similar symptoms of glare, halos, and starbursts around lights, ghosting or double images, and blurred vision that is difficult to describe (Erdinest et al, 2024).
Effective methods for quantifying HOAs rely on wavefront data from an aberrometer. This information can then be analyzed and incorporated into the optical design of a GP contact lens. The precision of these measurements relies on a high-quality scan through a mildly mydriatic pupil in a dark room, as well as a stable lens fit with minimal decentration and rotation. Patient selection is also paramount; this is a situation in which the practitioner must underpromise and hope to overdeliver.
There are uncontrollable factors such as neural adaptation to the wavefront correction, cataract development, and ocular surface disease that must be taken into account. But there is compelling evidence that HOA correction can be life-changing and drastically improve vision performance for the appropriate patients (Hastings et al, 2022; Gelles et al, 2022; Gelles et al, 2025).
HOAs are well-researched distortions that can impact nearly every patient to some degree. Optical correction of these distortions can be an answer to many patients’ concerns. As the measurement of HOAs and their correction with contact lenses become more accessible to general practice in the next decade, providers will have the potential to take vision to the next level.
References
1. Howland B, Howland HC. Subjective measurement of high-order aberrations of the eye. Science. 1976 Aug;193(4253):580-582. doi: 10.1126/science.959814
2. Liang J, Grimm B, Goelz S, Bille JF. Objective measurement of wave aberrations of the human eye with the use of a Hartmann-Shack wave-front sensor. J Opt Soc Am A Opt Image Sci Vis. 1994 Jul;11(7):1949-1957. doi: 10.1364/josaa.11.001949
3. McCormick GJ, Porter J, Cox IG, MacRae S. Higher-order aberrations in eyes with irregular corneas after laser refractive surgery. Ophthalmology. 2005 Oct;112(10):1699-1709. doi: 10.1016/j.ophtha.2005.04.022
4. Martínez-Pérez C, Santodomingo-Rubido J, Villa-Collar C, et al. Corneal higher-order aberrations in different types of irregular cornea. J Optom. 2024;17(4):100522. doi: 10.1016/j.optom.2024.100522
5. Erdinest N, London N, Landau D, et al. Higher order aberrations in keratoconus. Int Ophthalmol. 2024;44(1):172. doi: 10.1007/s10792-024-03118-5
6. Hastings GD, Nguyen LC, Kauffman MJ, Hemmati RT, Marsack JD, Applegate RA. Avoiding penetrating keratoplasty in severe keratoconus using a wavefront-guided scleral lens. Clin Exp Optom. 2022;105(1):86-88. doi: 10.1080/08164622.2021.1945407
7. Gelles JD, Cheung B, Akilov S, et al. Ocular impression-based scleral lens with wavefront-guided optics for visual improvement in keratoconus. Eye Contact Lens. 2022;48(11):485-488. doi: 10.1097/ICL.0000000000000922
8. Gelles JD, Su B, Kelly D, et al. Visual improvement with wavefront-guided scleral lenses for irregular corneal astigmatism. Eye Contact Lens. 2025;51(2):58-64. doi: 10.1097/ICL.0000000000001152