THE 8TH INTERNATIONAL FORUM FOR SCLERAL LENS RESEARCH (IFSLR), held in January 2025, convened experts from around the world to share and discuss emerging evidence and ongoing investigations in scleral lens (SL) research. The forum, scheduled just prior to the Global Specialty Lens Symposium (GSLS), serves as a focused platform for advancing research, fostering collaboration, and addressing knowledge gaps in the SL research field.
During 3 sessions, presenters covered foundational aspects of SL research, explored the physiological and pathological implications of SL wear, and highlighted innovative instrumentation and technology shaping future research and clinical practice. The following summaries provide key insights from each session.
Session I: So, You Want to Do Scleral Lens Research?
Three experts in clinical research led the first session of the 2025 IFSLR, which highlighted important considerations for study design, manuscript preparation, and regulatory compliance in SL research. Shehzad Naroo, MSc, PhD, editor-in-chief of Contact Lens & Anterior Eye, focused on the fundamentals of scientific writing and abstract preparation. He outlined the types of articles published in peer-reviewed literature, with most SL-related articles still being written as case reports and reviews, although research manuscripts are steadily increasing.
He outlined common pitfalls in manuscript preparation, including inadequate statistical reporting, lack of ethical oversight, and poorly defined research questions. He advised that abstracts must state concrete results and conclusions, avoiding vague phrases such as “results will be discussed.” Dr. Naroo also provided detailed recommendations on writing style, advocating for a third person, passive voice and structured presentation of methods, results, and figures to ensure reproducibility and reader comprehension.
Lyndon Jones, FCOptom, PhD, expanded on the practical challenges of conducting scleral lens research, drawing from his experience at the Centre for Ocular Research & Education (CORE) at the University of Waterloo. He emphasized the need for well-defined study objectives (ie, when assessing safety, visual outcomes, comfort, or usability) and selecting appropriate study designs (eg, randomized clinical trial, observational cohort).
In his talk, he highlighted the challenges of patient recruitment, especially in diverse populations such as those who have advanced keratoconus or systemic conditions causing severe dry eye. The variability in SL fitting techniques, lack of standardized outcome measures, and challenges with long-term follow-up were presented as major barriers to robust study design. However, Dr. Jones proposed some strategies to relieve some these challenges, such as leveraging specialty clinics, digital outreach, patient advocacy partnerships, and clinician training to improve recruitment, retention, and protocol consistency.
Meng Lin, OD, PhD, from University of California, Berkeley School of Optometry was the final speaker in the first session and addressed how to design a scientifically rigorous and ethical study protocol. She stressed the importance of well-formulated and precise research questions, as well as transparent communication of risks and benefits to study participants. She introduced the FINER (Feasible, Interesting, Novel, Ethical, Relevant) and PICO (Population, Intervention, Condition, Outcome) frameworks for generating testable hypotheses, emphasizing the importance of identifying the correct outcomes and confounding variables in SL studies.
Dr. Lin discussed the role of data safety monitoring boards for high-risk clinical trials and the essential function of institutional review boards (IRBs) in ensuring subject consent, safety, and data confidentiality. Additionally, she reviewed HIPAA considerations, encrypted data storage, and securing access to protect patient privacy.
Together, these speakers underscored the importance of study rigor, ethical guidelines, and methodology standardization in advancing SL research. Key themes of this session included the need for multidisciplinary collaboration, more defined success metrics, and alignment between clinical relevance and research design to improve the impact and reproducibility of SL studies.
Session II: Research on the Scleral Lens Impact on Health and Disease
The second session of the 2025 IFSLR, moderated by Karen DeLoss, OD, explored indications for SL beyond correcting irregular and regular refractive error. The first speaker, Sharon Qiu, OD, MS, from CORE at the University of Waterloo, reported on evidence in the literature addressing the question of whether SL wear could be helpful in managing patients with dry eye disease (DED) but lacking an irregular corneal surface (Qiu et al, 2024).
Currently, there are several published abstracts and paper presentations on this topic, including those that were published decades ago (Jacobs and Rosenthal, 2007; Kok and Visser, 1992; Rosenthal and Cotter, 2003), but there is a lack of evidence-based peer reviewed reports in support of this potentially useful option. Notably, she mentioned that SLs are currently listed in step 3 of DED management through the Tear Film & Ocular Surface Society Dry Eye Workshop II (TFOS DEWS II) treatment and management report (Jones et al, 2017). Although, she posited that using SLs earlier could be beneficial for many patients.
After discussing the many advantages of SLs in DED patients, namely the protective fluid barrier over the corneal surface, Dr. Qiu noted that some complications present in this population, often related to the tear fluid. For instance, not much is known about midday fogging in DED patients, although it appears to have a greater frequency in this population (Schornack et al, 2020). Furthermore, it was reported that the bigger bulk of SLs may be a significant wetting challenge for the DED patient.
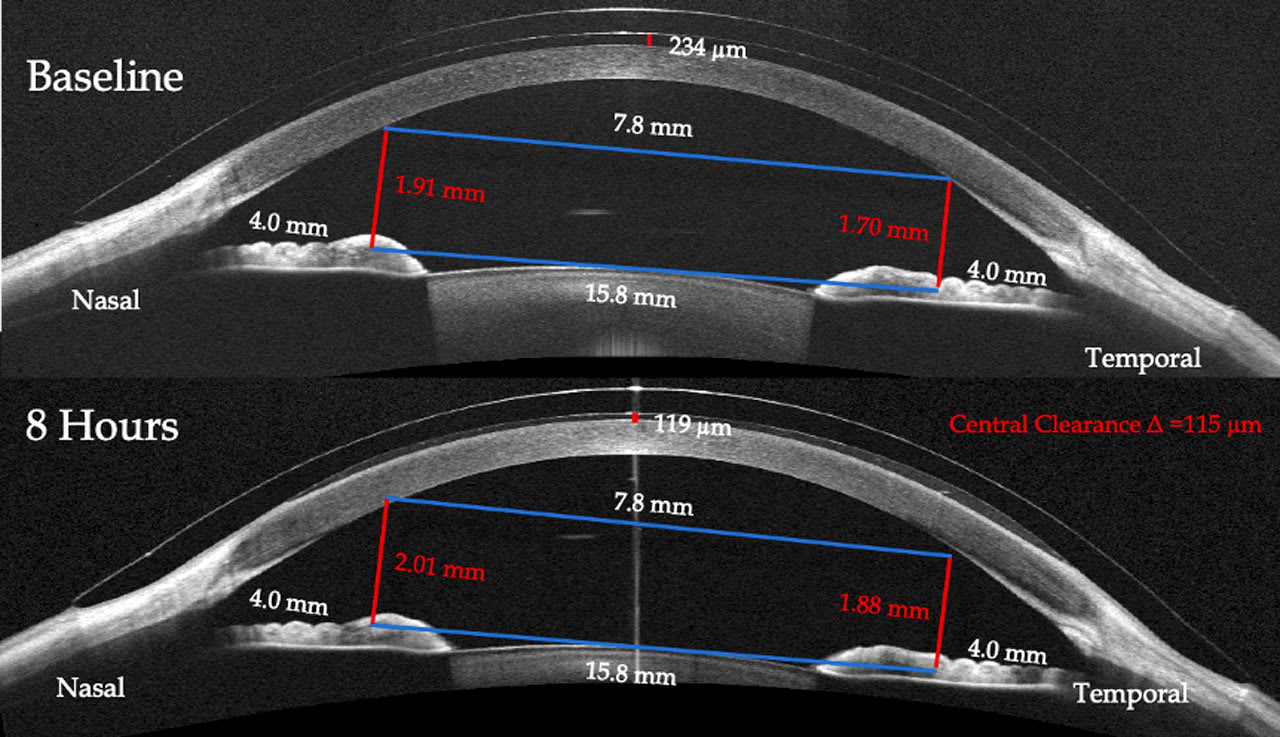
The second speaker in session II talked about instrument applications in SL care and presented some interesting data on SL settling. Josh Lotoczky, OD, at Michigan College of Optometry, illuminated SL settling with some exemplary anterior segment-optical coherence tomography (AS-OCT) images. OCT clearly demonstrated that the SL continues to settle over a long period of time (8 hours) and, in doing so, noticeably compresses the softer ocular surface tissue around limbus and conjunctiva. Interestingly, using a large-field AS-OCT, he was also able to evaluate the anterior chamber (AC) in the same images. Figure 1 shows that throughout the experimental period of 8 hours, the lenses settled into the soft conjunctiva, but the AC also became deeper, indicating that there was a force pulling the entire cornea more anteriorly. The continued settling over many hours may provide an argument for fitting lenses with a larger diameter to better vault the limbus.
One of the longstanding dilemmas in SL research is determining the impact of the devices upon intraocular pressure (IOP). With the current technology, it is essentially impossible to get a corneal IOP reading on an SL wearing eye. Langis Michaud, OD, MS, of the Université de Montréal, has taken an indirect route to overcome this dilemma and assessed the change in the optic nerve head Bruch’s membrane opening (BMO)-minimum rim width (MRW) as a surrogate for changing IOP. This approach of collecting data from the posterior pole rather than the anterior segment recorded a statistically significant change in the BMO-MRW ratio, which is suggestive of an IOP elevating capability of the SL.
This technique has been used in glaucoma studies and on normal eyes wearing SLs (Park et al, 2017; Samaha et al, 2021; Walker et al, 2020), and here was implemented in a study group of 14 adapted SL wearers with keratoconus (KC). The findings indicated thinning of the BMO-MRW (Michaud et al, 2025), which could infer an elevation in IOP. Although, Dr. Michaud noted that it is challenging to convert this directly to an IOP change. The KC cohort in this study showed a high intersubject variability, and there was no correlation with corneal biomechanics and their findings.
Dr. Michaud ended by discussing how this innovative approach still needs further testing and validation to allow direct IOP comparisons to BMO findings. But he noted that it appears that this technique could be a useful method in exploring changes in ocular health typically associated with changes in IOP.
Session III: Research on Scleral Lens Design, Instrumentation, and Technology
Technology plays an increasingly important role in specialty lens practice in general, and in SL practice in particular. The 3 presentations in the third and final session were great examples of some of the questions that we face in practice, and how instrumentation can help in research and in clinic to overcome these issues.
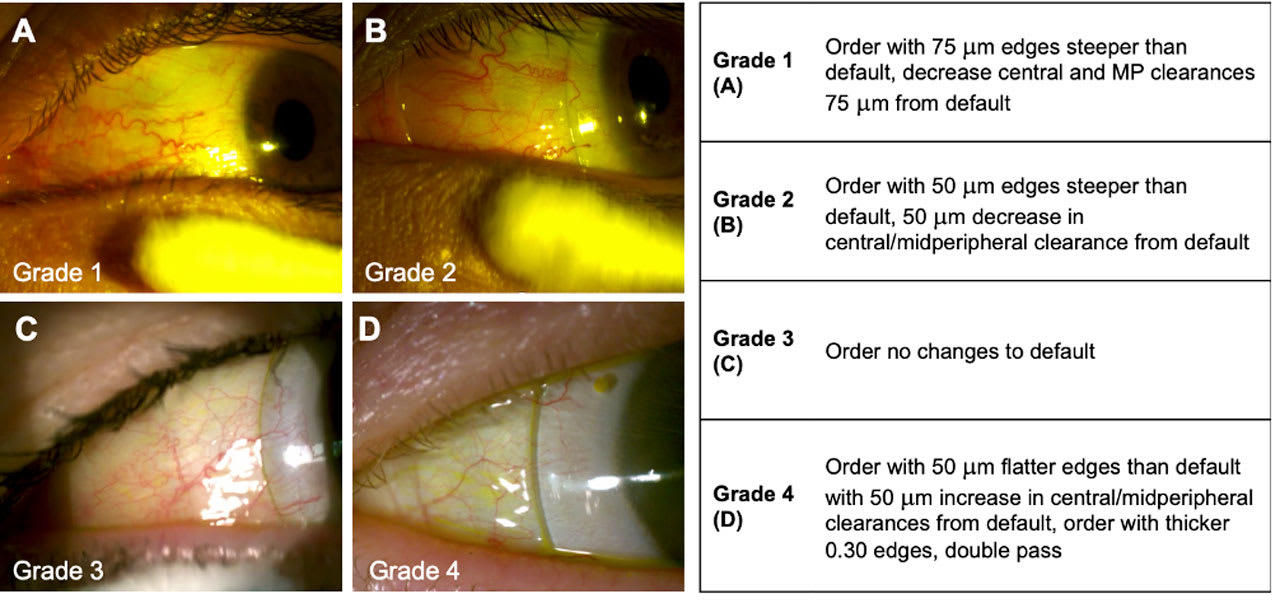
Caitlin Morrison, OD, discussed her techniques in a lecture titled “Cutting Down on Remakes by Grading Conjunctival Malleability.” Dr. Morrison, owner of In Focus: Specialty Contact Lens & Vision Solutions, observed different aspects of the conjunctival vessels of patients, and she has created a grading system that she uses when fitting SLs (Figure 2). Each grade corresponds with a specific “call to action” she follows to determine when ordering a lens order—ranging from “order a lens with 75 microns edges steeper than default, decrease central and midperipheral clearances by 75 microns from default,” to “order lens as usual” (no changes to default lens design).
The clinical applications of Hartman-Shack aberrometry devices in refractive surgery, intraocular lens, and contact lens corrections continues to grow. The need to compare the agreement and repeatability between devices is necessary. Daniel G. Fuller, OD, chief of the cornea contact lens service at the Southern College of Optometry, discussed his work looking at agreement between Pentacam AXL and Ovitz aberrometry. Both devices showed poor intrasession agreement on several measures, and there were no significant differences intraclass (ICC) and repeatability (RC) coefficients for devices except for ICC spherical aberration.
Pupil size is a key ingredient in aberrometry, he stated, and this needs further investigation for future studies, and for clinical application. Aberrometry seems to have huge potential, but the process of precise image capturing is challenging.
Rute Araújo, OD, PhD, from Portugal, presented the key findings of a study that evaluated meibomian gland alterations and validated a novel, quantitative method for their assessment (García-Marqués et al, 2022). The technique, which utilizes infrared meibography, allows for an objective and repeatable analysis of gland visibility, overcoming limitations of subjective grading scales.
Emphasis was placed on the essential role of meibomian glands in maintaining tear film stability and preventing dry eye symptoms. Their dysfunction, a leading cause of dry eye disease, highlights the clinical importance of accurate evaluation methods, particularly in SL wearers and potentially midday fogging. The study’s findings provide new insights into the structural and functional characteristics of meibomian glands over 1 year of scleral lens wear.
Conclusion
The 8th IFSLR showcased the potential for SLs to achieve greater impacts in areas such as DED. Innovative approaches to long-standing questions, such as the use of posterior segment imaging to evaluate ocular changes occurring during SL wear, continue to offer promising new methodologies to address unresolved concerns about SL safety, since the typical IOP measurements used by most clinicians are not possible during lens wear. The meeting also highlighted the role of aberrometry as a promising optical approach toward solving the visual problems resulting from higher-order aberrations due to postsurgical and pathological corneas, although image capturing instruments need further refining.
The planning for the 9th IFSLR is already underway with a focus on understanding global variation in SL utilization as well as research focused on disease and technology. This next meeting of the IFSLR will be held on January 7, 2026, and it will provide critical new findings and foster continued discussions on advancing research in the SL field.
Acknowledgement:The authors would like to acknowledge the SL researchers and clinicians that presented at the 8th annual IFSLR and provided content for this article; we would also like to acknowledge Drs. Gloria Chiu and Karen DeLoss who acted as moderators for the IFSLR sessions. Support for the 8th IFSLR was provided by Bausch Health, CooperVision, Contamac, Valley Contax, TruForm, and Visionary Optics. We appreciate the educational support from our media partners, Conexiant and the Global Specialty Lens Symposium, as well as our educational partner, The Scleral Lens Education Society.
References
1. Qiu SX, Fadel D, Hui A. Scleral lenses for managing dry eye disease in the absence of corneal irregularities: what is the current evidence? J Clin Med. 2024;13:3838. doi: 10.3390/jcm13133838
2. Jacobs DS, Rosenthal P. Boston scleral lens prosthetic device for treatment of severe dry eye in chronic graft-versus-host disease. Cornea. 2007;26(10):1195-1199. doi: 10.1097/ICO.0b013e318155743d
3. Kok JH, Visser R. Treatment of ocular surface disorders and dry eyes with high gas-permeable scleral lenses. Cornea. 1992;11(6):518-522. doi: 10.1097/00003226-199211000-00006
4. Rosenthal P, Cotter J. The Boston scleral lens in the management of severe ocular surface disease. Ophthalmol Clin North Am. 2003;16(1):89-93. doi: 10.1016/s0896-1549(02)00067-6
5. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575-628. doi: 10.1016/j.jtos.2017.05.006
6. Schornack MM, Fogt J, Harthan J, et al. Factors associated with patient-reported midday fogging in established scleral lens wearers. Cont Lens Anterior Eye. 2020;43(6): 602-608. doi: 10.1016/j.clae.2020.03.005
7. Park K, Kim J, Lee J. Reproducibility of Bruch membrane opening-minimum rim width measurements with spectral domain optical coherence tomography. J Glaucoma. 2017;26(11):1041-1050. doi: 10.1097/IJG.0000000000000787
8. Samaha D, Michaud L. Bruch membrane opening minimum rim width changes during scleral lens wear. Eye Contact Lens. 2021;47(5):295-300. doi: 10.1097/ICL.0000000000000750
9. Walker M, Pardon LP, Redfern R, Patel N. IOP and optic nerve head morphology during scleral lens wear. Optom Vis Sci. 2020;97(9):661-668. doi: 10.1097/OPX.0000000000001567
10. Michaud L, Balourdet S, Samaha D. Variation of Bruch’s membrane opening in response to intraocular pressure change during scleral lens wear, in a population with keratoconus. Ophthalmic Physiol Opt. 2025;45:405-415. doi: 10.1111/opo.13431
11. García-Marqués JV, Macedo-De-Araújo RJ, Cerviño A, García-Lázaro S, González-Méijome JM. Assessment of meibomian gland drop-out and visibility through a new quantitative method in scleral lens wearers: A one-year follow-up study. Cont Len Anterior Eye. 2023;46(1):101571. doi: 10.1016/j.clae.2021.101571